What triggers psoriasis?
Anais BambiliPsoriasis is a chronic inflammatory skin disease that affects millions of people worldwide. It manifests in various forms and can severely impact the quality of life of patients. Understanding the causes of psoriasis and the factors that trigger this disease is crucial for better managing and treating it. This article explores the triggers, types of psoriasis, and management strategies.
What is psoriasis?
Psoriasis is a chronic condition where skin cell renewal speeds up, leading to red patches covered with white scales. It is a chronic inflammatory disease in which the immune system plays a central role. This immune system imbalance causes excessive inflammation, which then speeds up the skin cell life cycle.

Accelerated Cell Cycle
The accelerated cell renewal in psoriasis is central to the formation of the red patches characteristic of this condition. Here's why it happens:
1. Normal Cell Cycle vs. Psoriasis
-
Normal Cycle: Normally, skin cells (keratinocytes) renew approximately every 28 to 30 days. Old, dead cells shed from the skin's surface and are replaced by new cells formed in the deeper layers.
-
Psoriasis Cycle: In people with psoriasis, this cycle is significantly accelerated. Skin cells renew in just 3 to 6 days. This means new skin cells reach the surface much faster than they should.
2. Skin Cell Buildup
-
Buildup: Due to this acceleration, skin cells don't have enough time to shed normally. They accumulate on the skin's surface, forming thick layers of immature cells.
-
Red Patches and Scales: This rapid cell buildup leads to thick, raised, reddish patches, often covered with silvery or white scales. These scales are actually dead cells that haven't been properly shed.
3. Inflammation
-
Inflammatory Response: The accumulation of skin cells triggers an inflammatory reaction in the skin. The immune system, which is imbalanced in psoriasis, mistakenly sends defense signals, believing it needs to fight an infection or attack.
-
Redness: This inflammation causes blood vessels in the skin to widen, leading to the characteristic redness of the patches. Immune cells also release pro-inflammatory substances, such as TNF-alpha and interleukins, which worsen inflammation and further accelerate the cell cycle.
4. Skin Thickening
-
Hyperproliferation: In addition to the buildup of dead cells, the new cells that rapidly rise to the surface don't have time to mature properly. They accumulate in thick layers, creating dense and rough patches.
-
Patch Texture: This hyperproliferation and chronic inflammation lead to thick, rough, and raised patches, which are often itchy and sometimes painful.
Causes of Psoriasis
The exact causes of psoriasis are not fully understood, but several factors are involved:
- Genetic Predisposition: People with psoriasis often have a genetic predisposition. If a parent has psoriasis, there is an increased risk for their children to develop the condition.
- Immune System: Psoriasis is largely due to a dysfunctional immune response. T-cells, a type of white blood cell, mistakenly attack healthy skin cells, causing inflammation and the rapid production of new skin cells.
- Trigger Factors: Various factors can trigger or worsen psoriasis, such as stress, infections (especially streptococcal infections which can trigger guttate psoriasis), skin trauma (Koebner phenomenon), certain medications, alcohol, and tobacco.
Different Types of Psoriasis
There are several types of psoriasis, each with specific characteristics:
-
Plaque Psoriasis: This is the most common form, characterized by thick, red patches covered with white or silvery scales. These patches often appear on the elbows, knees, scalp, and lower back.
-
Guttate Psoriasis: This appears as small, drop-shaped lesions on the skin, often triggered by a bacterial infection like strep throat.
-
Inverse Psoriasis: This type develops in skin folds, such as under the armpits, beneath the breasts, or in the groin area. The patches are often smooth and shiny.
-
Pustular Psoriasis: Characterized by non-infectious pustules surrounded by red skin, often found on the hands and feet.
-
Erythrodermic Psoriasis: This rare but severe form causes intense inflammation over a large part of the body's surface, requiring urgent medical attention.
Psoriasis and Psoriatic Arthritis
Around 30% of people with psoriasis develop psoriatic arthritis, a form of inflammatory arthritis that can cause joint pain, stiffness, and swelling. This complication highlights the importance of proactive disease management to prevent severe complications.
Managing Psoriasis
Psoriasis management depends on the severity of the condition and its impact on patients' quality of life. Treatments aim to reduce inflammation, slow down excessive skin cell production, and relieve symptoms.
-
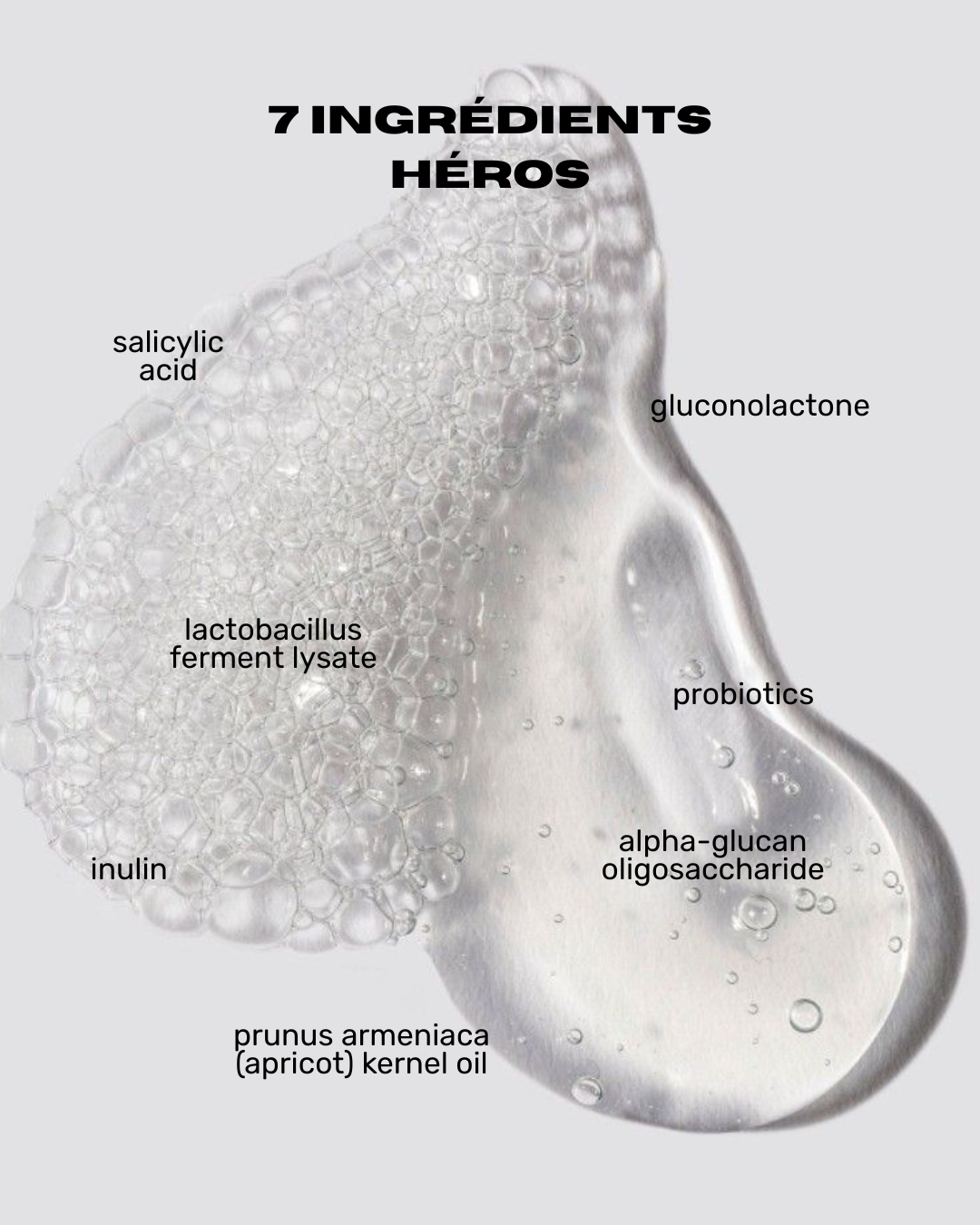
Topical Treatments: These include creams and ointments containing corticosteroids, vitamin D, or salicylic acid to reduce inflammation and skin thickening.
-
Phototherapy: Controlled exposure to ultraviolet B (UVB) rays can help reduce psoriasis symptoms, especially in moderate to severe cases.
-
Systemic Medications: For cases of severe psoriasis, systemic treatments like immunosuppressants or biologics may be prescribed to modulate the immune response.
-
Stress Management: Since stress is a major trigger, stress management techniques like meditation or behavioral therapy can be beneficial.
What Beauty Routine for Psoriasis?
A beauty routine adapted for psoriasis should be designed to soothe symptoms, hydrate the skin, and minimize irritation. Here is a recommended daily routine for people with psoriasis:
1. Gentle Cleansing
- Products to use: Opt for a gentle, soap-free cleanser, specially formulated for sensitive skin. Look for hypoallergenic, fragrance-free, and alcohol-free products that won't disrupt the skin's barrier.
- How: Wash your face and body with lukewarm water, never hot, as hot water can dry out the skin and worsen psoriasis patches.
2. Intense Hydration
- Products to use: Apply a thick moisturizing cream or balm containing ingredients such as ceramides, hyaluronic acid, shea butter, or natural oils like argan oil or avocado oil.
- How: Moisturize your skin immediately after showering, while it is still slightly damp. This helps to seal in moisture and protect the skin's barrier.

3. Targeted Treatments
- Products to use: If your dermatologist has prescribed topical creams (such as corticosteroids, retinoids, or vitamin D analogues), apply them to psoriasis patches after moisturizing. For over-the-counter treatments, products containing salicylic acid or coal tar can be effective in softening patches and reducing inflammation.
- How: Apply the treatment to affected areas, gently massaging until fully absorbed. Be sure to follow your dermatologist's instructions regarding frequency and amount to use.
4. Sun Protection
- Products to use: Use a broad-spectrum SPF 30 or higher, fragrance-free, non-comedogenic sunscreen to protect your skin from UV rays, which can worsen psoriasis symptoms in some people.
- How: Apply sunscreen generously to all exposed areas 15 minutes before going outside, and reapply every two hours if you are outdoors.
5. Exfoliation (Use with Caution)
- Products to use: Use a gentle scrub or a chemical exfoliant with lactic acid or salicylic acid to gently remove dead skin cells, but avoid mechanical scrubs that can irritate the skin.
- How: Limit exfoliation to once or twice a week and be gentle. If your skin is very sensitive or experiencing a flare-up, it's best to skip this step.

6. Soothing Bath or Shower
- Products to use: Add natural oils like colloidal oatmeal or Epsom salts to your bath to soothe your skin.
- How: Don't stay in the water for too long (no more than 10-15 minutes) to prevent skin dryness. After bathing, gently pat your skin dry with a towel instead of rubbing.
7. Avoid Irritants
- What to avoid: Avoid products containing fragrances, dyes, parabens, or alcohol, as they can irritate the skin. Choose soft cotton clothing and avoid rough or synthetic fabrics that can cause friction.
8. Scalp Care
- Products to use: Use a medicated shampoo containing salicylic acid, coal tar, or zinc sulfate to treat scalp psoriasis.
- How: Gently massage the shampoo into your scalp and leave it on for a few minutes before rinsing. Avoid scratching the patches, even if they are itchy.
9. Stress Management
- Why: Stress is a major trigger for psoriasis. Incorporate stress management techniques into your daily routine, such as meditation, yoga, or deep breathing exercises.
10. Regular Consultation with a Dermatologist
- Why: A dermatologist can adjust your skincare routine based on how your psoriasis is progressing, prescribe specific treatments, and monitor for potential side effects.
Conclusion
Psoriasis is a complex condition resulting from the interaction between genetic predisposition, the immune system, and various triggering factors. While living with psoriasis can be challenging, appropriate management, including tailored psoriasis treatments and proactive symptom management, can significantly improve patients' quality of life. If you experience symptoms of psoriasis, it's important to consult a healthcare professional for a diagnosis and a personalized treatment plan.