What are the effects of hormones on the body and skin?
Anais BambiliStarling's original definition of a hormone in 1905 was: "a hormone is a substance produced by internal secretion glands, which serve to transmit signals through the blood to target organs".
Today, new definitions also do not fully encompass the meaning of hormones as specific information carriers. A major issue is the lack of distinction between hormones and other signaling molecules such as cytokines, growth factors, or autacoid compounds.
However, it seems that a precise definition may not even be possible, as some cytokines and growth factors act as hormones under certain conditions!
In this article, we will focus on recognized hormones, which are essential chemical messengers that govern the complex functioning of the human body.
Released by the endocrine glands, these substances play a central role in regulating and coordinating physiological functions. To deeply explore the effects of hormones on the body, we examine and explain the different hormone categories and their specific impact.

-
Sex Hormones: Pillars of Reproduction
Sex hormones, including estrogen and progesterone in women, and testosterone in men, are crucial for the development of secondary sexual characteristics.
Secondary sexual characteristics are distinct physical traits that develop during puberty and differentiate male and female individuals of a species. These characteristics are not directly related to reproduction, unlike primary sexual characteristics such as genitals, but they play an essential role in signaling sexual maturity.
Secondary sexual characteristics emerge under the influence of sex hormones, mainly estrogen and progesterone in women, and testosterone in men.
In women:
- Breast development: Under the influence of estrogen, mammary glands develop, leading to breast formation. This is one of the first visible signs of puberty in girls.
- Growth of pubic and armpit hair: Sex hormones stimulate hair growth in the pubic region and under the armpits, signaling the onset of puberty.
- Body fat distribution: Estrogen influences fat distribution, often leading to an increase in fat mass around the hips and thighs.
- Hip widening: Puberty often leads to a widening of the pelvis, contributing to the characteristic female silhouette.
- Onset of the menstrual cycle: The onset of menstruation is a key secondary sexual characteristic, marking the potential for reproduction.

In men:
- Breast growth: Although less pronounced than in women, a small amount of breast tissue can develop in men during puberty.
- Facial and body hair growth: Testosterone stimulates hair growth on the face, legs, torso, and other body areas.
- Shoulder and jaw widening: Testosterone promotes muscle development, often leading to wider shoulders and a more defined jawline.
- Adam's apple growth: A cartilaginous protrusion called the Adam's apple becomes more pronounced in men during puberty.
- Genital enlargement: Puberty induces the growth of external genitals, including the penis and testicles.
- Voice change: Testosterone causes the vocal cords to thicken, leading to a significant lowering of the voice during puberty.
Secreted by the ovaries and testicles, sex hormones regulate the menstrual cycle, spermatogenesis (the process of sperm development), and are therefore essential for reproduction. In women, the ovaries produce estrogen and progesterone, regulating puberty, ovulation, and the menstrual cycle.
-
Thyroid Hormones: Architects of Metabolism
Thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3), secreted by the thyroid gland, orchestrate metabolism. They influence energy consumption, growth, and organ development, ensuring hormonal balance and proper body function. Thyroid hormones are also essential for brain development during gestation.

-
Peptide Hormones: Rapid Regulators
Peptide hormones, such as insulin and adrenaline, are released by the pancreas and adrenal glands. They regulate glucose metabolism, stress response, and other bodily processes. The pancreas, through insulin, controls blood sugar levels, while the adrenal glands produce adrenaline, triggering the 'fight or flight' response during acute stress.
-
Derived Hormones: Specific Origins
Some hormones, like melatonin produced by the pineal gland, have unique origins. They influence the circadian rhythm, regulating sleep and wakefulness. These derived hormones, often linked to the nervous system, demonstrate the wide variety of hormonal sources in the human body.
-
Endocrine Gland: The Master of Hormones
Endocrine glands, including the thyroid, adrenal glands, and pancreas, are responsible for the secretion and release of hormones. As the command center for hormones, they constantly adjust hormone levels to meet the body's physiological needs.
The hypothalamus and pituitary gland, key components of the endocrine system, regulate hormone secretion and maintain hormonal balance.
-
Growth Hormone: Development Accelerator
Growth hormone, produced by the pituitary gland, stimulates the growth and development of tissues. It plays a crucial role in children's growth and tissue regeneration in adults. This stimulation of growth primarily occurs during deep sleep.

-
Steroid Hormones: Key Players in the Endocrine System
Steroid hormones, such as cortisol and sex hormones, are derived from cholesterol. Secreted by the adrenal glands and gonads, they regulate various functions, from stress response to metabolism. Sex hormones, like testosterone, are responsible for the development of secondary sexual characteristics.
-
Hormone Therapy and Gender Transition
Transgender individuals have a gender identity that differs from the sex they were assigned at birth. For many transgender people, access to gender-affirming hormone therapy (GAHT) is an important and medically necessary step in their gender transition.
For trans men, masculinizing hormone therapy involves testosterone treatment. Testosterone can be administered via injections under the skin or into the muscle, by applying gel, or through a skin solution. Sometimes, other hormonal treatments may be prescribed.
For trans women, feminizing hormone therapy consists of:
- Anti-androgens, taken as tablets and more rarely by injection, to reduce male hormones.
- Estrogens
- Progesterone
The choice of treatment is made based on the doctor's recommendations and the patient's preferences. There is no evidence that one approved method of administering treatment is more effective than another.

What are the physical effects of hormones?
Hormones induce physical changes that align with one's gender identity.
Most changes are observed over a 2-year period. The speed and quality of these changes vary from person to person.
Feminizing and masculinizing regimens are safe when used within established hormonal protocols and are associated with significant improvements in mental health outcomes, including reduced depression, anxiety, and gender dysphoria.
What are the effects of hormone therapy on the skin?
The effects on the skin vary depending on the type of transition and the hormone therapy chosen.
Hormone therapy can lead to two main effects on your skin:
- An epidermis that produces fewer lipids, meaning less oil: the skin becomes drier, and issues related to oily or combination skin (blackheads, adult acne, etc.) tend to decrease. This often happens when male hormones are inhibited in favor of female hormones;
- Or, conversely, an increased production of sebum, linked to a rise in male hormones in the body. The skin thickens, becomes oilier, and imperfections may appear.
For trans men, increased hair growth can lead to ingrown hair problems: the skin becomes red locally, inflammation occurs, and in some cases, a small hard bump appears under the skin.
How to care for your skin during gender transition?
The beauty routine generally remains the same:
- Cleanse your skin twice a day to remove impurities
- Moisturize your face with a product suited to skin changes: a rich cream for dry skin, and a mattifying anti-blemish cream for skin that becomes oily.
- Once or twice a week, use a scrub and a purifying exfoliating mask to stimulate cell renewal and refine skin texture.
You can prioritize certain active ingredients:
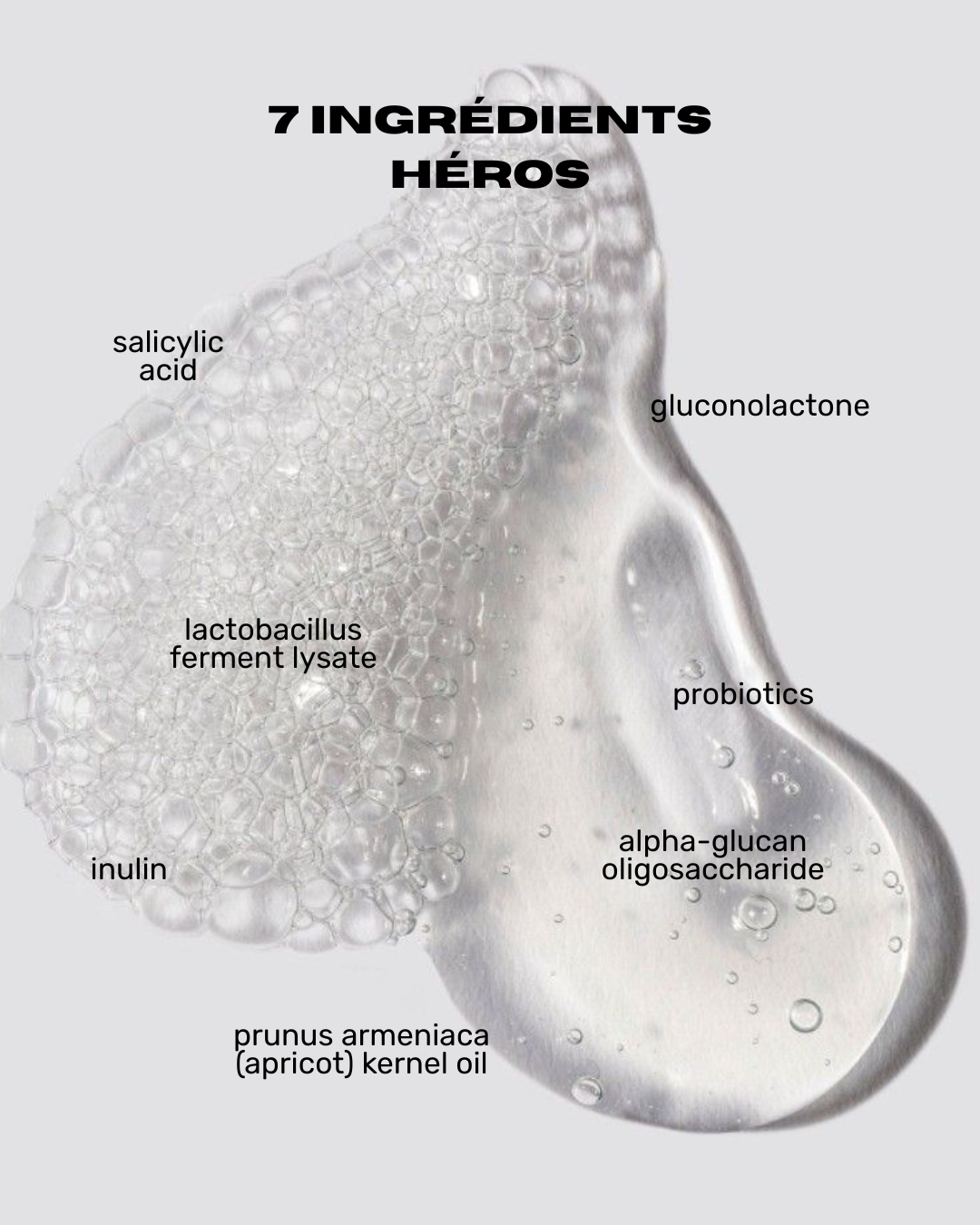
- Salicylic acid for its immediate exfoliating action on the stratum corneum, which reduces the number of imperfections.
- Zinc gluconate to regulate sebum production upstream, reduce shine, and eliminate blackheads.
For dry skin, apply a cream rich in lipids and ceramides.
-
Hormone Replacement Therapy
Hormone Replacement Therapy (HRT) involves supplementing women with hormones lost during the menopausal transition. To relieve symptoms associated with menopause, conventional HRT includes an estrogen and progesterone component to mimic hormones produced by the human ovary. Many estrogen-based therapies exist, including those naturally present in the human ovary, such as estradiol and estriol. Other estrogenic compounds include conjugated equine estrogen (CEE), the most commonly prescribed estrogen in the United States. They are not identical in their effect on the human body but share the same FDA indications.
Conclusion
Hormones, the regulators of homeostasis, orchestrate a sophisticated ballet within the human body. Each category of hormones, whether sex, thyroid, peptide, derived, endocrine, growth, or steroid, uniquely contributes to maintaining physiological balance. The secretion, stimulation, and reception by hormone receptors are crucial elements in this complex chemical dance, illustrating the subtlety of hormonal regulation. This in-depth understanding is essential to appreciate the sophistication of the endocrine systems and their implications for overall health.
Sources
1. Unger CA. Hormone therapy for transgender patients. Transl Androl Urol. 2016 Dec;5(6):877-884. doi: 10.21037/tau.2016.09.04. PMID: 28078219; PMCID: PMC5182227.
2. Harper-Harrison G, Shanahan MM. Hormone Replacement Therapy. 2023 Feb 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 29630243.
3. Stárka L, Dušková M. What is a hormone? Physiol Res. 2020 Sep 30;69(Suppl 2):S183-S185. doi: 10.33549/physiolres.934509. PMID: 33094616; PMCID: PMC8603735.