Atopic dermatitis | symptoms, causes, treatment
Share
Skin diseases are common and can vary in terms of symptoms, severity and triggers. Among these skin conditions, atopic dermatitis, often confused witheczema, is a chronic inflammatory skin disease that affects a significant number of people, both children and the adult population. In this article, we'll explore in detail what atopic dermatitis is, the differences between eczema and atopic dermatitis, its causes, and how to prevent and treat it effectively.
What is atopic dermatitis?
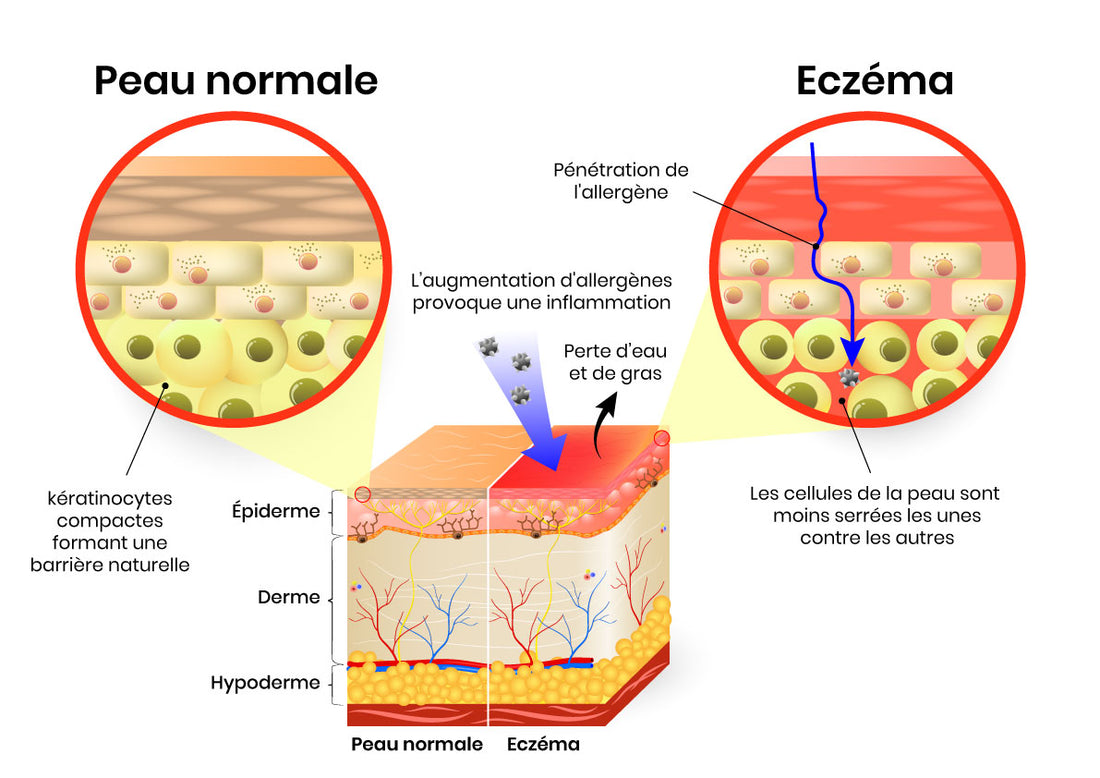
Atopic dermatitis, also known asatopic eczema, is an inflammatory skin disease characterized byitching, redness and rashes. This condition affects the skin barrier, making it less effective at retaining moisture and protecting the skin from external aggressors. As a result, people with atopic dermatitis often have dry skin, and are more prone to inflammation and skin infections.
Symptoms of atopic dermatitis
The symptoms of atopic dermatitis vary according to the age of the sufferer. Infants may present with rashes on the face, scalp, cheeks and other parts of the body. In older children and adults, rashes may appear on the folds of the elbows and knees, as well as on the neck, hands and feet.
People with atopic dermatitis generally have atopic skin, which means they have an impaired skin barrier. The skin barrier is a protective layer of the skin that maintains hydration and prevents irritants and allergens from penetrating. In people with atopic dermatitis, this barrier is compromised, resulting in moisture loss and increased sensitivity.
The main symptoms of atopic dermatitis include:
- Intense itching
- Skin redness
- Dry, flaky skin
- Formation of vesicles or scabs
- Skin thickening
- Increased sensitivity to various irritants
Atopic dermatitis is a chronic disease, which means it can recur throughout a person's life. Symptoms can be aggravated by triggers such as stress, food allergies, skin infections or seasonal changes.
What is the difference between eczema and atopic dermatitis?
The term "eczema" is often used interchangeably with "atopic dermatitis", but it's important to note that eczema is a broader term that encompasses a variety of inflammatory skin conditions. Atopic dermatitis is one of the most common types of eczema, but there are other forms with significant differences.
- The different types of eczema
Atopic dermatitis (atopic eczema): As described above, atopic dermatitis is a chronic inflammatory skin disease characterized by itching, redness and rashes. It is often linked to a family history of the disease and to environmental factors.
- Contact eczema: Contact eczema is a skin reaction caused by direct contact with an irritating or allergenic substance, such as chemicals, metals, cosmetics or plants.
- Nummular eczema: Nummular eczema manifests itself as round or oval patches of inflamed, scaly skin. Unlike atopic dermatitis, it is not necessarily associated with a family history or allergies.
- Dyshidrosic eczema: Dyshidrosic eczema mainly affects the hands and feet, causing the formation of small fluid-filled vesicles. It is often painful and can be triggered by stress.
- Allergic contact dermatitis: Allergic contact dermatitis is a skin reaction caused by an allergy to a specific substance, such as nickel or rubber.
Differences in symptoms between eczema and atopic dermatitis
The symptoms of atopic dermatitis and eczema can sometimes overlap, but there are distinctive features that help differentiate them. Atopic dermatitis is characterized by intense itching, red rashes and lesions, while contact eczema can cause localized rashes at the site of contact with the irritating or allergenic substance.
It's essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan, as treatment for each type of eczema can vary.

Causes of atopic dermatitis
Atopic dermatitis is a complex disease whose exact causes are not yet fully understood. However, there are several known factors that contribute to the development of this skin condition.
- Genetic predisposition
Genetics is one of the key factors in atopic dermatitis. A family history of the disease increases an individual's risk of developing the condition. Studies have identified certain genes linked to atopic dermatitis, underlining the importance of hereditary factors in its development.
- Environmental factors
Although genetics play a major role, environmental factors can also trigger or aggravate atopic dermatitis. These factors include:
- Food allergies: Food allergies, particularly in infants and young children, can contribute to the development of atopic dermatitis. However, it's important to note that atopic dermatitis is not itself an allergy.
- Hay fever and allergic rhinitis: Hay fever and allergic rhinitis sufferers have an increased risk of developing atopic dermatitis.
- Eating habits: A diet rich in processed foods, sugar and dairy products can aggravate the symptoms of atopic dermatitis in some people.
How is atopic dermatitis treated?
Treatment of atopic dermatitis aims to reduce symptoms, prevent flare-ups and improve the patient's quality of life. The treatment plan may vary depending on the severity of the disease, the patient's age and other individual factors. Here are some commonly used treatment approaches:
- Skin care
Skin care is essential for managing atopic dermatitis. Recommendations include:
- Use mild, fragrance-free cleansers to avoid skin irritation.
- Apply emollient moisturizers to keep skin hydrated.
- Avoid hot showers and baths, preferring lukewarm water.
- Gently dry skin after bathing rather than rubbing.
- Topical medications
In cases of more severe atopic dermatitis, doctors may prescribe topical medications such as corticosteroids or calcineurin inhibitors. These drugs help reduce inflammation and relieve itching.
- Oral medications
In the event of severe or persistent flare-ups, oral medications such as oral corticosteroids or immunosuppressive drugs may be prescribed by a healthcare professional.
- Biological therapies
Biological therapies are drugs that modify the immune system and can be used in cases of severe atopic dermatitis that do not respond to other treatments.
- Preventing triggers
Avoiding known triggers is essential to prevent flare-ups of atopic dermatitis. This can include managing stress, identifying and avoiding food allergens, and protecting against environmental irritants.
- Allergy management
For people with atopic dermatitis associated with food allergies, management of these allergies is crucial. Consulting an allergist for allergy testing and an appropriate management plan is recommended.
Conclusion
Atopic dermatitis, also known asatopic eczema, is an inflammatory skindisease that can have a significant impact on the quality of life of those affected. Understanding the differences between eczema and atopic dermatitis, as well as the factors contributing to its development, is essential for accurate diagnosis and effective treatment.
While there is no definitive cure for atopic dermatitis, many treatment options are available to relieve symptoms and prevent flare-ups. It is advisable to consult a healthcare professional for a diagnosis and personalized treatment plan. In addition, managing triggers, good skin hygiene and preventing food allergies can play a key role in managing this chronic skin condition.